Search
- Page Path
- HOME > Search
- Miscellaneous
- Immune Checkpoint Inhibitors and Endocrine Disorders: A Position Statement from the Korean Endocrine Society
- Hyemi Kwon, Eun Roh, Chang Ho Ahn, Hee Kyung Kim, Cheol Ryong Ku, Kyong Yeun Jung, Ju Hee Lee, Eun Heui Kim, Sunghwan Suh, Sangmo Hong, Jeonghoon Ha, Jun Sung Moon, Jin Hwa Kim, Mi-kyung Kim, The Committee of Clinical Practice Guideline of the Korean Endocrine Society
- Endocrinol Metab. 2022;37(6):839-850. Published online December 26, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1627
- 3,524 View
- 321 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
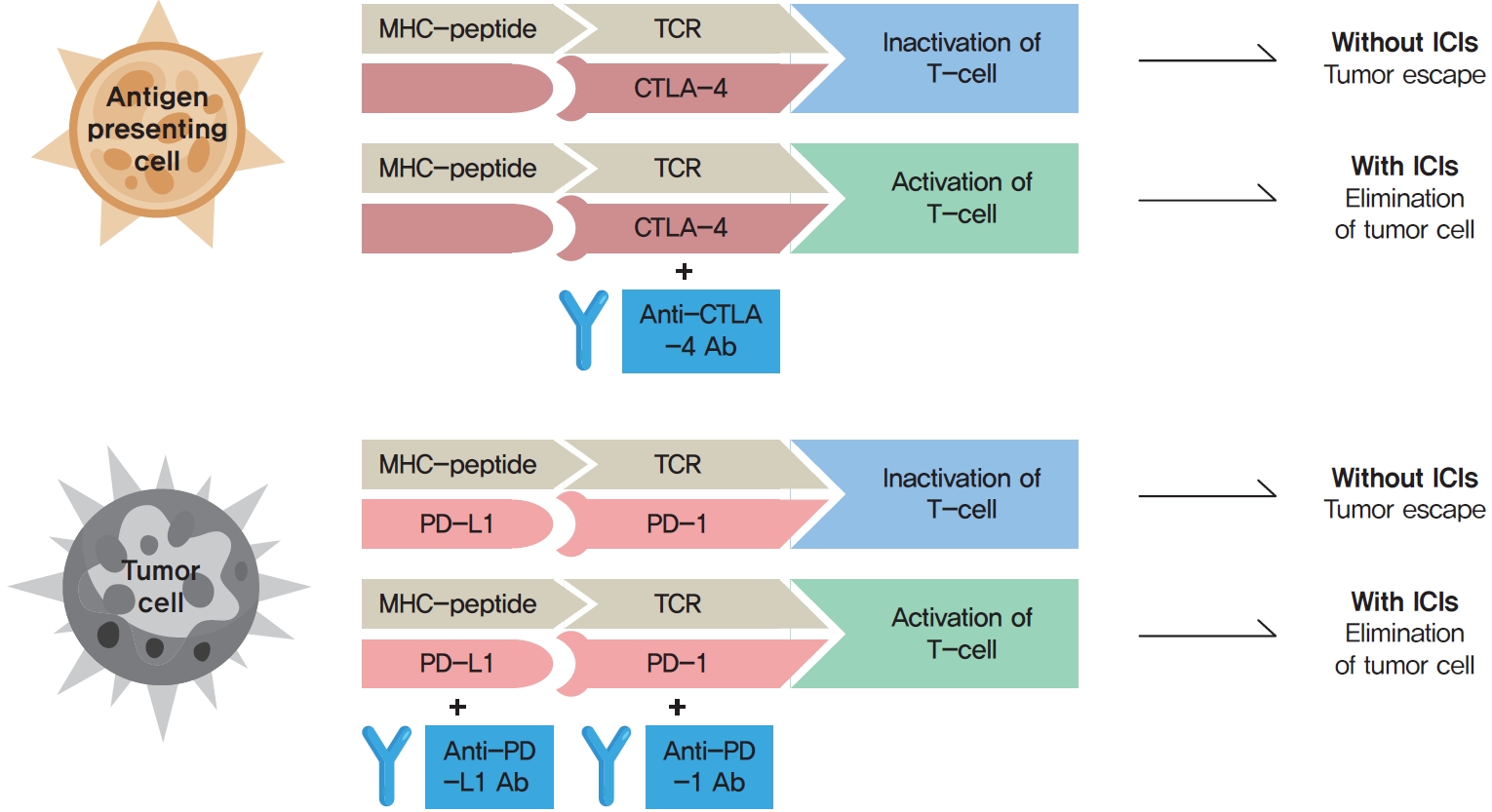
ePub - Immune checkpoint inhibitors (ICIs) including an anti-cytotoxic T-lymphocyte-associated antigen 4 inhibitor, anti-programmed cell death protein 1 (PD-1) inhibitors, and anti-PD-ligand 1 inhibitors are representative therapeutics for various malignancies. In oncology, the application of ICIs is currently expanding to a wider range of malignancies due to their remarkable clinical outcomes. ICIs target immune checkpoints which suppress the activity of T-cells that are specific for tumor antigens, thereby allowing tumor cells to escape the immune response. However, immune checkpoints also play a crucial role in preventing autoimmune reactions. Therefore, ICIs targeting immune checkpoints can trigger various immune-related adverse events (irAEs), especially in endocrine organs. Considering the endocrine organs that are frequently involved, irAEs associated endocrinopathies are frequently life-threatening and have unfavorable clinical implications for patients. However, there are very limited data from large clinical trials that would inform the development of clinical guidelines for patients with irAEs associated endocrinopathies. Considering the current clinical situation, in which the scope and scale of the application of ICIs are increasing, position statements from clinical specialists play an essential role in providing the appropriate recommendations based on both medical evidence and clinical experience. As endocrinologists, we would like to present precautions and recommendations for the management of immune-related endocrine disorders, especially those involving the adrenal, thyroid, and pituitary glands caused by ICIs.
-
Citations
Citations to this article as recorded by- Pembrolizumab plus lenvatinib for radically unresectable or metastatic renal cell carcinoma in the Japanese population
Ryo Fujiwara, Takeshi yuasa, kenichi kobayashi, tetsuya yoshida, susumu kageyama
Expert Review of Anticancer Therapy.2023; 23(5): 461. CrossRef - Incidence of Endocrine-Related Dysfunction in Patients Treated with New Immune Checkpoint Inhibitors: A Meta-Analysis and Comprehensive Review
Won Sang Yoo, Eu Jeong Ku, Eun Kyung Lee, Hwa Young Ahn
Endocrinology and Metabolism.2023; 38(6): 750. CrossRef
- Pembrolizumab plus lenvatinib for radically unresectable or metastatic renal cell carcinoma in the Japanese population

- Miscellaneous
- COVID-19 Vaccination for Endocrine Patients: A Position Statement from the Korean Endocrine Society
- Cheol Ryong Ku, Kyong Yeun Jung, Chang Ho Ahn, Jun Sung Moon, Ju Hee Lee, Eun Heui Kim, Hyemi Kwon, Hee Kyung Kim, Sunghwan Suh, Sangmo Hong, Jeonghoon Ha, Eun Roh, Jin Hwa Kim, Mi-kyung Kim, the Committee of Clinical Practice Guideline of the Korean Endocrine Society
- Endocrinol Metab. 2021;36(4):757-765. Published online August 17, 2021
- DOI: https://doi.org/10.3803/EnM.2021.404
- 10,386 View
- 419 Download
- 19 Web of Science
- 21 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Since the first outbreak of coronavirus disease 2019 (COVID-19), ongoing efforts have been made to discover an efficacious vaccine against COVID-19 to combat the pandemic. In most countries, both mRNA and DNA vaccines have been administered, and their side effects have also been reported. The clinical course of COVID-19 and the effects of vaccination against COVID-19 are both influenced by patients’ health status and involve a systemic physiological response. In view of the systemic function of endocrine hormones, endocrine disorders themselves and the therapeutics used to treat them can influence the outcomes of vaccination for COVID-19. However, there are very limited data to support the development of clinical guidelines for patients with specific medical backgrounds based on large clinical trials. In the current severe circumstances of the COVID-19 pandemic, position statements made by clinical specialists are essential to provide appropriate recommendations based on both medical evidence and clinical experiences. As endocrinologists, we would like to present the medical background of COVID-19 vaccination, as well as precautions to prevent the side effects of COVID-19 vaccination in patients with specific endocrine disorders, including adrenal insufficiency, diabetes mellitus, osteoporosis, autoimmune thyroid disease, hypogonadism, and pituitary disorders.
-
Citations
Citations to this article as recorded by- COVID-19 mRNA vaccine may trigger subacute thyroiditis
Mehmet Sözen, Ömercan Topaloğlu, Berrin Çetinarslan, Alev Selek, Zeynep Cantürk, Emre Gezer, Damla Köksalan, Taner Bayraktaroğlu
Human Vaccines & Immunotherapeutics.2024; 17(12): 5120. CrossRef - The role of co-morbidities in the development of an AEFI after COVID-19 vaccination in a large prospective cohort with patient-reported outcomes in the Netherlands
C. Ouaddouh, J.W. Duijster, T. Lieber, F.P.A.M. van Hunsel
Expert Opinion on Drug Safety.2024; 23(3): 323. CrossRef - Thyroid dysfunction in COVID-19
David Tak Wai Lui, Chi Ho Lee, Yu Cho Woo, Ivan Fan Ngai Hung, Karen Siu Ling Lam
Nature Reviews Endocrinology.2024;[Epub] CrossRef - Adult-Onset Type 1 Diabetes Development Following COVID-19 mRNA Vaccination
Hyeyeon Moon, Sunghwan Suh, Mi Kyoung Park
Journal of Korean Medical Science.2023;[Epub] CrossRef - Prior immunization status of COVID-19 patients and disease severity: A multicenter retrospective cohort study assessing the different types of immunity
Javaria Aslam, Faisal Shahzad Khan, Muhammad Talha Haris, Hewad Hewadmal, Maryam Khalid, Mohammad Y. Alshahrani, Qurrat-ul-ain Aslam, Irrum Aneela, Urooj Zafar
Vaccine.2023; 41(2): 598. CrossRef - Mortality and Severity of Coronavirus Disease 2019 in Patients with Long-Term Glucocorticoid Therapy: A Korean Nationwide Cohort Study
Eu Jeong Ku, Keeho Song, Kyoung Min Kim, Gi Hyeon Seo, Soon Jib Yoo
Endocrinology and Metabolism.2023; 38(2): 253. CrossRef - Pituitary Diseases and COVID-19 Outcomes in South Korea: A Nationwide Cohort Study
Jeonghoon Ha, Kyoung Min Kim, Dong-Jun Lim, Keeho Song, Gi Hyeon Seo
Journal of Clinical Medicine.2023; 12(14): 4799. CrossRef - Inactivated SARS-CoV-2 vaccination does not disturb the clinical course of Graves’ disease: An observational cohort study
Shichen Xu, Huixin Yu, Xian Cheng, Jing Wu, Jiandong Bao, Li Zhang
Vaccine.2023; 41(38): 5648. CrossRef - Adrenal Crisis Associated With COVID-19 Vaccination in Patients With Adrenal Insufficiency
Yukako Kurematsu, Takako Mohri, Sadanori Okada, Yutaka Takahashi
JCEM Case Reports.2023;[Epub] CrossRef - Adverse Events Associated with COVID-19 Vaccination in Adolescents with Endocrinological Disorders: A Cross-Sectional Study
İbrahim Mert Erbaş, İrem Ceren Erbaş, Gözde Akın Kağızmanlı, Kübra Yüksek Acinikli, Özge Besci, Korcan Demir, Ece Böber, Nurşen Belet, Ayhan Abacı
Journal of Clinical Research in Pediatric Endocrinology.2023; 15(3): 248. CrossRef - Neue Aspekte der Glukokortikoidsubstitution bei Nebennierenrindeninsuffizienz
Tina Kienitz, Gesine Meyer
Der Internist.2022; 63(1): 12. CrossRef - Endocrine Follow-up During Post-Acute COVID-19: Practical Recommendations Based on Available Clinical Evidence
Rimesh Pal, Ameya Joshi, Sanjay K. Bhadada, Mainak Banerjee, Suresh Vaikkakara, Satinath Mukhopadhyay
Endocrine Practice.2022; 28(4): 425. CrossRef - Safety of Inactivated and mRNA COVID-19 Vaccination Among Patients Treated for Hypothyroidism: A Population-Based Cohort Study
Xi Xiong, Carlos King Ho Wong, Ivan Chi Ho Au, Francisco Tsz Tsun Lai, Xue Li, Eric Yuk Fai Wan, Celine Sze Ling Chui, Esther Wai Yin Chan, Franco Wing Tak Cheng, Kristy Tsz Kwan Lau, Chi Ho Lee, Yu Cho Woo, David Tak Wai Lui, Ian Chi Kei Wong
Thyroid.2022; 32(5): 505. CrossRef - The New Entity of Subacute Thyroiditis amid the COVID-19 Pandemic: From Infection to Vaccine
Mihaela Popescu, Adina Ghemigian, Corina Maria Vasile, Andrei Costache, Mara Carsote, Alice Elena Ghenea
Diagnostics.2022; 12(4): 960. CrossRef - Adrenal Crisis Secondary to COVID-19 Vaccination in a Patient With Hypopituitarism
Nikolina Markovic, Anila Faizan, Chirag Boradia, Sridhar Nambi
AACE Clinical Case Reports.2022; 8(4): 171. CrossRef - The Effect of Inactivated SARS-CoV-2 Vaccines on TRAB in Graves’ Disease
LingHong Huang, ZhengRong Jiang, JingXiong Zhou, YuPing Chen, HuiBin Huang
Frontiers in Endocrinology.2022;[Epub] CrossRef - Osteoporosis in Patients With Respiratory Diseases
Yue Ma, Shui Qiu, Renyi Zhou
Frontiers in Physiology.2022;[Epub] CrossRef - Pilot Findings on SARS-CoV-2 Vaccine-Induced Pituitary Diseases: A Mini Review from Diagnosis to Pathophysiology
Ach Taieb, El Euch Mounira
Vaccines.2022; 10(12): 2004. CrossRef - Forty Years Together, New Leap Forward! The 40th Anniversary of the Korean Endocrine Society
Jong Chul Won, Ki-Hyun Baek
Endocrinology and Metabolism.2022; 37(6): 851. CrossRef - No need of glucocorticoid dose adjustment in patients with adrenal insufficiency before COVID-19 vaccine
Tania Pilli, Cristina Dalmiglio, Gilda Dalmazio, Alfonso Sagnella, Raffaella Forleo, Lucia Brilli, Fabio Maino, Cristina Ciuoli, Maria Grazia Castagna
European Journal of Endocrinology.2022; 187(1): K7. CrossRef - Diabetes and COVID-19 Vaccination
Hae Dong Choi, Jun Sung Moon
The Journal of Korean Diabetes.2021; 22(4): 221. CrossRef
- COVID-19 mRNA vaccine may trigger subacute thyroiditis

- Diabetes, Obesity and Metabolism
- Expression of LONP1 Is High in Visceral Adipose Tissue in Obesity, and Is Associated with Glucose and Lipid Metabolism
- Ju Hee Lee, Saet-Byel Jung, Seong Eun Lee, Ji Eun Kim, Jung Tae Kim, Yea Eun Kang, Seul Gi Kang, Hyon-Seung Yi, Young Bok Ko, Ki Hwan Lee, Bon Jeong Ku, Minho Shong, Hyun Jin Kim
- Endocrinol Metab. 2021;36(3):661-671. Published online June 22, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1023
- 4,507 View
- 151 Download
- 7 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
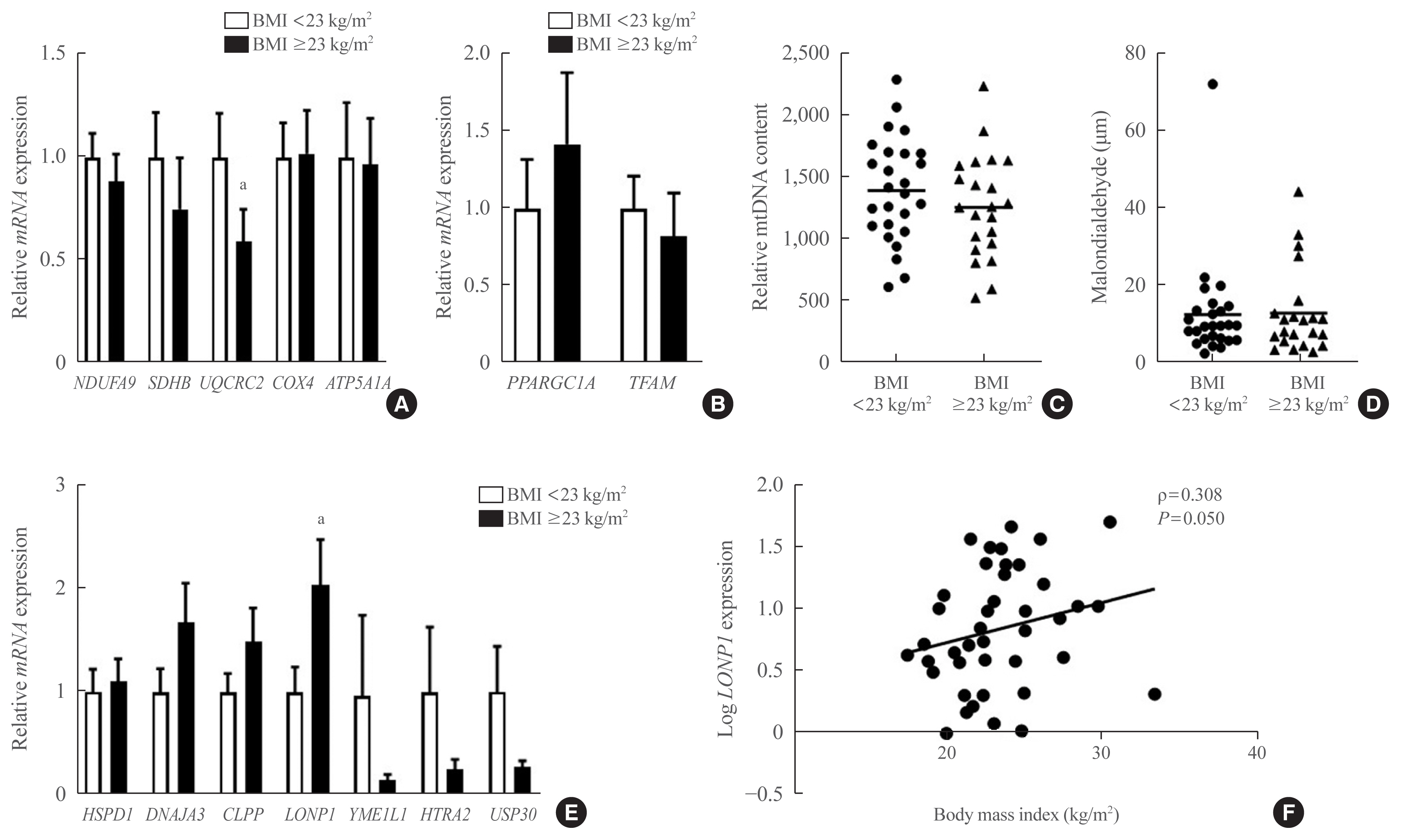
The nature and role of the mitochondrial stress response in adipose tissue in relation to obesity are not yet known. To determine whether the mitochondrial unfolded protein response (UPRmt) in adipose tissue is associated with obesity in humans and rodents.
Methods
Visceral adipose tissue (VAT) was obtained from 48 normoglycemic women who underwent surgery. Expression levels of mRNA and proteins were measured for mitochondrial chaperones, intrinsic proteases, and components of electron-transport chains. Furthermore, we systematically analyzed metabolic phenotypes with a large panel of isogenic BXD inbred mouse strains and Genotype-Tissue Expression (GTEx) data.
Results
In VAT, expression of mitochondrial chaperones and intrinsic proteases localized in inner and outer mitochondrial membranes was not associated with body mass index (BMI), except for the Lon protease homolog, mitochondrial, and the corresponding gene LONP1, which showed high-level expression in the VAT of overweight or obese individuals. Expression of LONP1 in VAT positively correlated with BMI. Analysis of the GTEx database revealed that elevation of LONP1 expression is associated with enhancement of genes involved in glucose and lipid metabolism in VAT. Mice with higher Lonp1 expression in adipose tissue had better systemic glucose metabolism than mice with lower Lonp1 expression.
Conclusion
Expression of mitochondrial LONP1, which is involved in the mitochondrial quality control stress response, was elevated in the VAT of obese individuals. In a bioinformatics analysis, high LONP1 expression in VAT was associated with enhanced glucose and lipid metabolism. -
Citations
Citations to this article as recorded by- LONP1 ameliorates liver injury and improves gluconeogenesis dysfunction in acute-on-chronic liver failure
Muchen Wu, Jing Wu, Kai Liu, Minjie Jiang, Fang Xie, Xuehong Yin, Jushan Wu, Qinghua Meng
Chinese Medical Journal.2024; 137(2): 190. CrossRef - Mitochondrial quality control proteases and their modulation for cancer therapy
Jiangnan Zhang, Wenliang Qiao, Youfu Luo
Medicinal Research Reviews.2023; 43(2): 399. CrossRef - Effects of Obesity and Calorie Restriction on Cancer Development
Ekaterina Sergeeva, Tatiana Ruksha, Yulia Fefelova
International Journal of Molecular Sciences.2023; 24(11): 9601. CrossRef - Mitochondrial Dysfunction Associated with mtDNA in Metabolic Syndrome and Obesity
Natalia Todosenko, Olga Khaziakhmatova, Vladimir Malashchenko, Kristina Yurova, Maria Bograya, Maria Beletskaya, Maria Vulf, Natalia Gazatova, Larisa Litvinova
International Journal of Molecular Sciences.2023; 24(15): 12012. CrossRef - Down‐regulation of Lon protease 1 lysine crotonylation aggravates mitochondrial dysfunction in polycystic ovary syndrome
Yuan Xie, Shuwen Chen, Zaixin Guo, Ying Tian, Xinyu Hong, Penghui Feng, Qiu Xie, Qi Yu
MedComm.2023;[Epub] CrossRef - The mitochondrial unfolded protein response: A multitasking giant in the fight against human diseases
Zixin Zhou, Yumei Fan, Ruikai Zong, Ke Tan
Ageing Research Reviews.2022; 81: 101702. CrossRef
- LONP1 ameliorates liver injury and improves gluconeogenesis dysfunction in acute-on-chronic liver failure

- Miscellaneous
- Diagnosis and Treatment of Growth Hormone Deficiency: A Position Statement from Korean Endocrine Society and Korean Society of Pediatric Endocrinology
- Jung Hee Kim, Hyun Wook Chae, Sang Ouk Chin, Cheol Ryong Ku, Kyeong Hye Park, Dong Jun Lim, Kwang Joon Kim, Jung Soo Lim, Gyuri Kim, Yun Mi Choi, Seong Hee Ahn, Min Ji Jeon, Yul Hwangbo, Ju Hee Lee, Bu Kyung Kim, Yong Jun Choi, Kyung Ae Lee, Seong-Su Moon, Hwa Young Ahn, Hoon Sung Choi, Sang Mo Hong, Dong Yeob Shin, Ji A Seo, Se Hwa Kim, Seungjoon Oh, Sung Hoon Yu, Byung Joon Kim, Choong Ho Shin, Sung-Woon Kim, Chong Hwa Kim, Eun Jig Lee
- Endocrinol Metab. 2020;35(2):272-287. Published online June 24, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.2.272
- 9,507 View
- 429 Download
- 14 Web of Science
- 16 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
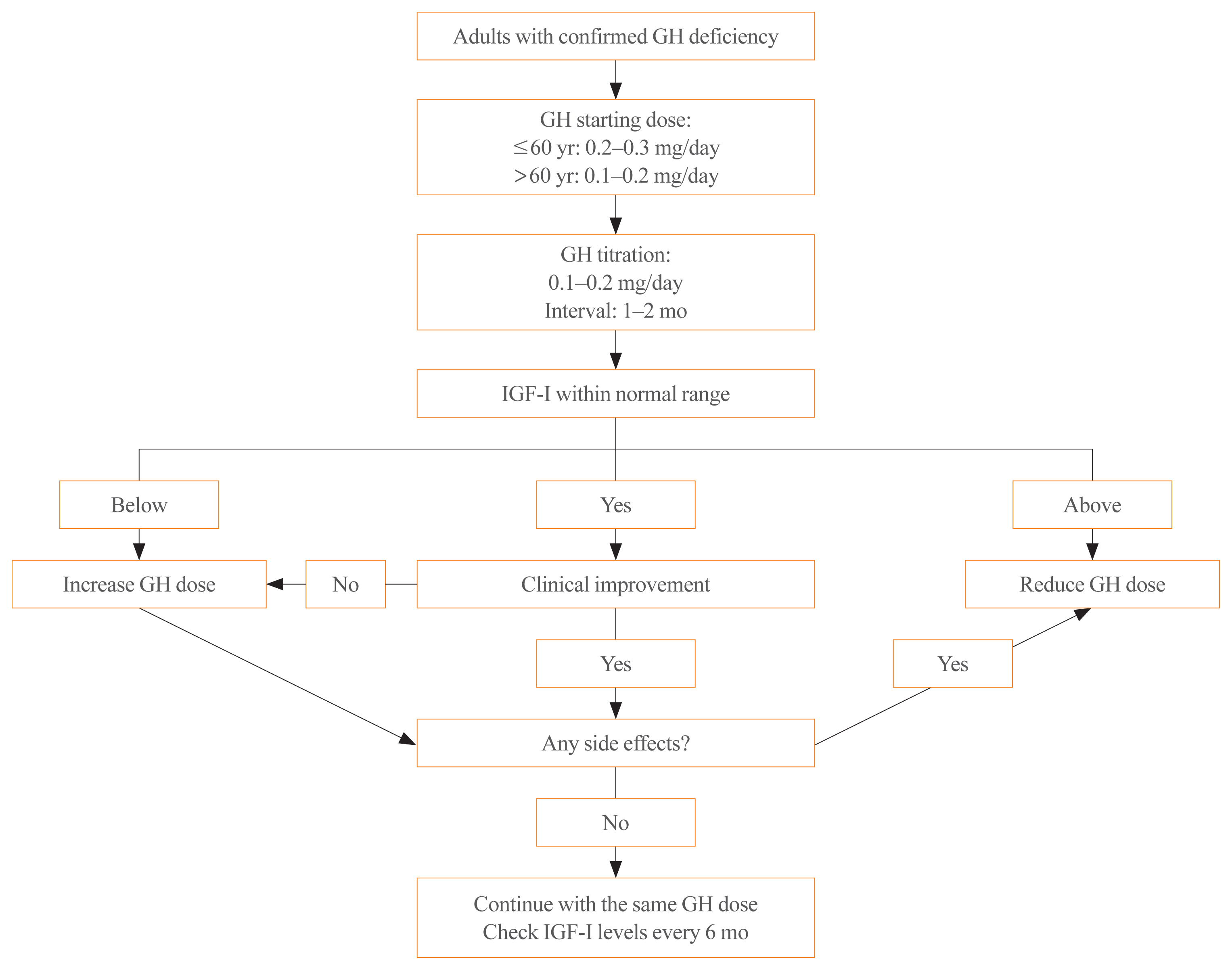
ePub - Growth hormone (GH) deficiency is caused by congenital or acquired causes and occurs in childhood or adulthood. GH replacement therapy brings benefits to body composition, exercise capacity, skeletal health, cardiovascular outcomes, and quality of life. Before initiating GH replacement, GH deficiency should be confirmed through proper stimulation tests, and in cases with proven genetic causes or structural lesions, repeated GH stimulation testing is not necessary. The dosing regimen of GH replacement therapy should be individualized, with the goal of minimizing side effects and maximizing clinical improvements. The Korean Endocrine Society and the Korean Society of Pediatric Endocrinology have developed a position statement on the diagnosis and treatment of GH deficiency. This position statement is based on a systematic review of evidence and expert opinions.
-
Citations
Citations to this article as recorded by- Once-Weekly Somapacitan as an Alternative Management of Growth Hormone Deficiency in Prepubertal Children: A Systematic Review and Meta-Analysis of Randomized Controlled Trial
Ghina Tsurayya, Cut Alifiya Nazhifah, Muhammad Rahmat Pirwanja, Putri Oktaviani Zulfa, Muhammad Raihan Ramadhan Tatroman, Fajar Fakri, Muhammad Iqhrammullah
Children.2024; 11(2): 227. CrossRef - Efficacy, safety, and patient satisfaction of norditropin and sogroya in patients with growth hormone deficiency: a systematic review and meta-analysis of randomized controlled trials
Obieda Altobaishat, Mohamed Abouzid, Mostafa Hossam El Din Moawad, Abdulrahman Sharaf, Yazan Al-Ajlouni, Tungki Pratama Umar, Abdallah Bani-salameh, Mohammad Tanashat, Omar Abdullah Bataineh, Abdulqadir J. Nashwan
Endocrine.2024;[Epub] CrossRef - Evaluation of Adult Height in Patients with Non-Permanent Idiopathic GH Deficiency
Agnese Murianni, Anna Lussu, Chiara Guzzetti, Anastasia Ibba, Letizia Casula, Mariacarolina Salerno, Marco Cappa, Sandro Loche
Endocrines.2023; 4(1): 169. CrossRef - The effect of hypothalamic involvement and growth hormone treatment on cardiovascular risk factors during the transition period in patients with childhood-onset craniopharyngioma
Sang Hee Park, Yun Jeong Lee, Jung-Eun Cheon, Choong Ho Shin, Hae Woon Jung, Young Ah Lee
Annals of Pediatric Endocrinology & Metabolism.2023; 28(2): 107. CrossRef - Continuous Glucose Monitoring: A Possible Aid for Detecting Hypoglycemic Events during Insulin Tolerance Tests
Soo Yeun Sim, Moon Bae Ahn
Sensors.2023; 23(15): 6892. CrossRef - The risk patients with AGHD have of developing CVD
Eisha Javed, Maha Zehra, Naz Elahi
International Journal of Cardiology Cardiovascular Risk and Prevention.2023; 19: 200221. CrossRef - Diagnosis of GH Deficiency Without GH Stimulation Tests
Anastasia Ibba, Sandro Loche
Frontiers in Endocrinology.2022;[Epub] CrossRef - Metabolic Impacts of Discontinuation and Resumption of Recombinant Human Growth Hormone Treatment during the Transition Period in Patients with Childhood-Onset Growth Hormone Deficiency
Yun Jeong Lee, Yunha Choi, Han-Wook Yoo, Young Ah Lee, Choong Ho Shin, Han Saem Choi, Ho-Seong Kim, Jae Hyun Kim, Jung Eun Moon, Cheol Woo Ko, Moon Bae Ahn, Byung-Kyu Suh, Jin-Ho Choi
Endocrinology and Metabolism.2022; 37(2): 359. CrossRef - A Radiomics-Based Model with the Potential to Differentiate Growth Hormone Deficiency and Idiopathic Short Stature on Sella MRI
Taeyoun Lee, Kyungchul Song, Beomseok Sohn, Jihwan Eom, Sung Soo Ahn, Ho-Seong Kim, Seung-Koo Lee
Yonsei Medical Journal.2022; 63(9): 856. CrossRef - Phenotypic spectrum of patients with mutations in CHD7: clinical implications of endocrinological findings
Ja Hye Kim, Yunha Choi, Soojin Hwang, Gu-Hwan Kim, Han-Wook Yoo, Jin-Ho Choi
Endocrine Connections.2022;[Epub] CrossRef - Immune Checkpoint Inhibitors and Endocrine Disorders: A Position Statement from the Korean Endocrine Society
Hyemi Kwon, Eun Roh, Chang Ho Ahn, Hee Kyung Kim, Cheol Ryong Ku, Kyong Yeun Jung, Ju Hee Lee, Eun Heui Kim, Sunghwan Suh, Sangmo Hong, Jeonghoon Ha, Jun Sung Moon, Jin Hwa Kim, Mi-kyung Kim
Endocrinology and Metabolism.2022; 37(6): 839. CrossRef - Laron syndrome: clinic, diagnostics (а clinical case)
P.M. Lіashuk, R.P. Lіashuk, N.I. Stankova, M.B. Kudina
INTERNATIONAL JOURNAL OF ENDOCRINOLOGY (Ukraine).2022; 18(3): 193. CrossRef - Diagnosis for Pheochromocytoma and Paraganglioma: A Joint Position Statement of the Korean Pheochromocytoma and Paraganglioma Task Force
Eu Jeong Ku, Kyoung Jin Kim, Jung Hee Kim, Mi Kyung Kim, Chang Ho Ahn, Kyung Ae Lee, Seung Hun Lee, You-Bin Lee, Kyeong Hye Park, Yun Mi Choi, Namki Hong, A Ram Hong, Sang-Wook Kang, Byung Kwan Park, Moon-Woo Seong, Myungshin Kim, Kyeong Cheon Jung, Chan
Endocrinology and Metabolism.2021; 36(2): 322. CrossRef - Asian Conference on Tumor Ablation Guidelines for Adrenal Tumor Ablation
Byung Kwan Park, Masashi Fujimori, Shu-Huei Shen, Uei Pua
Endocrinology and Metabolism.2021; 36(3): 553. CrossRef - Asian Conference on Tumor Ablation guidelines for renal cell carcinoma
Byung Kwan Park, Shu-Huei Shen, Masashi Fujimori, Yi Wang
Investigative and Clinical Urology.2021; 62(4): 378. CrossRef - Diagnosis and Treatment of Adult Growth Hormone Deficiency
Jung Hee Kim
The Korean Journal of Medicine.2021; 96(5): 400. CrossRef
- Once-Weekly Somapacitan as an Alternative Management of Growth Hormone Deficiency in Prepubertal Children: A Systematic Review and Meta-Analysis of Randomized Controlled Trial

- Clinical Study
- Genetic Analysis of CLCN7 in an Old Female Patient with Type II Autosomal Dominant Osteopetrosis
- Seon Young Kim, Younghak Lee, Yea Eun Kang, Ji Min Kim, Kyong Hye Joung, Ju Hee Lee, Koon Soon Kim, Hyun Jin Kim, Bon Jeong Ku, Minho Shong, Hyon-Seung Yi
- Endocrinol Metab. 2018;33(3):380-386. Published online September 18, 2018
- DOI: https://doi.org/10.3803/EnM.2018.33.3.380
- 4,196 View
- 58 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background Type II autosomal dominant osteopetrosis (ADO II) is a rare genetically heterogeneous disorder characterized by osteosclerosis and increased bone mass, predominantly involving spine, pelvis, and skull. It is closely related to functional defect of osteoclasts caused by chloride voltage-gated channel 7 (
CLCN7 ) gene mutations. In this study, we aimed to identify the pathogenic mutation in a Korean patient with ADO II using whole exome sequencing.Methods We evaluated the clinical, biochemical, and radiographic analysis of a 68-year-old woman with ADO II. We also performed whole exome sequencing to identify pathogenic mutation of a rare genetic disorder of the skeleton. Moreover, a polymorphism phenotyping program, Polymorphism Phenotyping v2 (PolyPhen-2), was used to assess the effect of the identified mutation on protein function.
Results Whole exome sequencing using peripheral leukocytes revealed a heterozygous c.296A>G missense mutation in the
CLCN7 gene. The mutation was also confirmed using Sanger sequencing. The mutation c.296A>G was regarded to have a pathogenic effect by PolyPhen-2 software.Conclusion We detect a heterozygous mutation in
CLCN7 gene of a patient with ADO II, which is the first report in Korea. Our present findings suggest that symptoms and signs of ADO II patient having a c.296A>G mutation inCLCN7 may appear at a very late age. The present study would also enrich the database ofCLCN7 mutations and improve our understanding of ADO II.-
Citations
Citations to this article as recorded by- Autosomal dominant osteopetrosis type II resulting from a de novo mutation in the CLCN7 gene: A case report
Xiu-Li Song, Li-Yuan Peng, Dao-Wen Wang, Hong Wang
World Journal of Clinical Cases.2022; 10(20): 6936. CrossRef - Magnetic resonance findings in a Cavalier King Charles spaniel with osteopetrosis, Chiari‐like malformation and syringomyelia
Ricardo Fernandes, C J Jordan, Colin Driver
Veterinary Record Case Reports.2019;[Epub] CrossRef
- Autosomal dominant osteopetrosis type II resulting from a de novo mutation in the CLCN7 gene: A case report

- Clinical Study
- The Role of Circulating Slit2, the One of the Newly Batokines, in Human Diabetes Mellitus
- Yea Eun Kang, Sorim Choung, Ju Hee Lee, Hyun Jin Kim, Bon Jeong Ku
- Endocrinol Metab. 2017;32(3):383-388. Published online September 18, 2017
- DOI: https://doi.org/10.3803/EnM.2017.32.3.383
- 3,865 View
- 52 Download
- 19 Web of Science
- 17 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Slit2 is a new secreted protein from adipose tissue that improves glucose hemostasis in mice; however, there is no study about the serum levels and precise role of Slit2 in human. The aim of this study is to explore the serum level of Slit2 in human, and to identify the role of Slit2 in diabetes mellitus (DM).
Methods The participants of this study consist of 38 subjects with newly diagnosed DM, and 75 healthy subjects as a control group. Serum Slit2 levels were measured using an enzyme-linked immunosorbent assay. Relationship between circulating Slit2 and diabetic related factors was investigated in diabetic group compared with non-diabetic group. Additionally, the correlations between the serum level of Slit2 and diverse metabolic parameters were analyzed.
Results Circulating Slit2 level was more decreased in diabetic group than in control group, but there was no significant difference statistically. Interestingly, serum levels of Slit2 were significantly negatively correlated to the serum concentrations of fasting glucose (coefficient
r =–0.246,P =0.008), the serum concentrations of postprandial glucose (coefficientr =–0.233,P =0.017), and glycosylated hemoglobin (HbA1c; coefficientr =–0.357,P <0.001).Conclusion From our study, the first report of circulating Slit2 levels in human, circulating Slit2 level significantly negatively correlated with serum glucose and HbA1c. Our results suggest that the circulating Slit2 may play a role in maintainence of glucose homeostasis in human, even though exact contribution and mechanism are not yet known.
-
Citations
Citations to this article as recorded by- Brown adipose tissue-derived metabolites and their role in regulating metabolism
Khanyisani Ziqubu, Phiwayinkosi V. Dludla, Sihle E. Mabhida, Babalwa U. Jack, Susanne Keipert, Martin Jastroch, Sithandiwe E. Mazibuko-Mbeje
Metabolism.2024; 150: 155709. CrossRef - An update on the secretory functions of brown, white, and beige adipose tissue: Towards therapeutic applications
Zeinab Ghesmati, Mohsen Rashid, Shabnam Fayezi, Frank Gieseler, Effat Alizadeh, Masoud Darabi
Reviews in Endocrine and Metabolic Disorders.2024; 25(2): 279. CrossRef - The integrated bioinformatic analysis identifies immune microenvironment-related potential biomarkers for patients with gestational diabetes mellitus
Jie-ling Chen, Hui-fang Dai, Xin-chen Kan, Jie Wu, Hong-Wu Chen
Frontiers in Immunology.2024;[Epub] CrossRef - Adipokines from white adipose tissue in regulation of whole body energy homeostasis
Bijayashree Sahu, Naresh C. Bal
Biochimie.2023; 204: 92. CrossRef - The Role of Slit-2 in Gestational Diabetes Mellitus and Its Effect on Pregnancy Outcome
Yan Wang, Shihua Zhao, Wei Peng, Ying Chen, Jingwei Chi, Kui Che, Yangang Wang
Frontiers in Endocrinology.2022;[Epub] CrossRef - The Heartwarming Effect of Brown Adipose Tissue
Kelsey M. Pinckard, Kristin I. Stanford
Molecular Pharmacology.2022; 102(1): 39. CrossRef - New players of the adipose secretome: Therapeutic opportunities and challenges
Laetitia Coassolo, Niels Banhos Dannieskiold-Samsøe, Meng Zhao, Hobson Allen, Katrin J. Svensson
Current Opinion in Pharmacology.2022; 67: 102302. CrossRef - Serum CD14 concentration is associated with obesity and insulin resistance in non-diabetic individuals
Yea Eun Kang, Kyong Hye Joung, Ji Min Kim, Ju Hee Lee, Hyun Jin Kim, Bon Jeong Ku
Journal of International Medical Research.2022; 50(10): 030006052211300. CrossRef - Brown/Beige adipose tissues and the emerging role of their secretory factors in improving metabolic health: The batokines
Bilal Ahmad, Muhammad Sufyan Vohra, Mansab Ali Saleemi, Christopher J. Serpell, Isabel Lim Fong, Eng Hwa Wong
Biochimie.2021; 184: 26. CrossRef - Thermogenic Fat: Development, Physiological Function, and Therapeutic Potential
Bruna B. Brandão, Ankita Poojari, Atefeh Rabiee
International Journal of Molecular Sciences.2021; 22(11): 5906. CrossRef - Brown Adipose Crosstalk in Tissue Plasticity and Human Metabolism
Camilla Scheele, Christian Wolfrum
Endocrine Reviews.2020; 41(1): 53. CrossRef - Development of a Cell-Based Assay for the Detection of Neutralizing Antibodies to PF-06730512 Using Homogenous Time-Resolved Fluorescence
Michael Luong, Ying Wang, Stephen P. Berasi, Janet E. Buhlmann, Hongying Yang, Boris Gorovits
The AAPS Journal.2020;[Epub] CrossRef - Brown and beige fat: From molecules to physiology and pathophysiology
Stefania Carobbio, Anne-Claire Guénantin, Isabella Samuelson, Myriam Bahri, Antonio Vidal-Puig
Biochimica et Biophysica Acta (BBA) - Molecular and Cell Biology of Lipids.2019; 1864(1): 37. CrossRef - Serum R-Spondin 1 Is a New Surrogate Marker for Obesity and Insulin Resistance
Yea Eun Kang, Ji Min Kim, Hyon-Seung Yi, Kyong Hye Joung, Ju Hee Lee, Hyun Jin Kim, Bon Jeong Ku
Diabetes & Metabolism Journal.2019; 43(3): 368. CrossRef - Deletion of Robo4 prevents high‐fat diet‐induced adipose artery and systemic metabolic dysfunction
Tam T. T. Phuong, Ashley E. Walker, Grant D. Henson, Daniel R. Machin, Dean Y. Li, Anthony J. Donato, Lisa A. Lesniewski
Microcirculation.2019;[Epub] CrossRef - Adipose Tissue-Derived Signatures for Obesity and Type 2 Diabetes: Adipokines, Batokines and MicroRNAs
Min-Woo Lee, Mihye Lee, Kyoung-Jin Oh
Journal of Clinical Medicine.2019; 8(6): 854. CrossRef - The role of brown and beige adipose tissue in glycaemic control
Katarina Klepac, Anastasia Georgiadi, Matthias Tschöp, Stephan Herzig
Molecular Aspects of Medicine.2019; 68: 90. CrossRef
- Brown adipose tissue-derived metabolites and their role in regulating metabolism

- Clinical Study
- The Eosinophil Count Tends to Be Negatively Associated with Levels of Serum Glucose in Patients with Adrenal Cushing Syndrome
- Younghak Lee, Hyon-Seung Yi, Hae Ri Kim, Kyong Hye Joung, Yea Eun Kang, Ju Hee Lee, Koon Soon Kim, Hyun Jin Kim, Bon Jeong Ku, Minho Shong
- Endocrinol Metab. 2017;32(3):353-359. Published online September 18, 2017
- DOI: https://doi.org/10.3803/EnM.2017.32.3.353
- 7,700 View
- 46 Download
- 6 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Cushing syndrome is characterized by glucose intolerance, cardiovascular disease, and an enhanced systemic inflammatory response caused by chronic exposure to excess cortisol. Eosinopenia is frequently observed in patients with adrenal Cushing syndrome, but the relationship between the eosinophil count in peripheral blood and indicators of glucose level in patients with adrenal Cushing syndrome has not been determined.
Methods A retrospective study was undertaken of the clinical and laboratory findings of 40 patients diagnosed with adrenal Cushing syndrome at Chungnam National University Hospital from January 2006 to December 2016. Clinical characteristics, complete blood cell counts with white blood cell differential, measures of their endocrine function, description of imaging studies, and pathologic findings were obtained from their medical records.
Results Eosinophil composition and count were restored by surgical treatment of all of the patients with adrenal Cushing disease. The eosinophil count was inversely correlated with serum and urine cortisol, glycated hemoglobin, and inflammatory markers in the patients with adrenal Cushing syndrome.
Conclusion Smaller eosinophil populations in patients with adrenal Cushing syndrome tend to be correlated with higher levels of blood sugar and glycated hemoglobin. This study suggests that peripheral blood eosinophil composition or count may be associated with serum glucose levels in patients with adrenal Cushing syndrome.
-
Citations
Citations to this article as recorded by- Association between Eosinophil Count and Cortisol Concentrations in Equids Admitted in the Emergency Unit with Abdominal Pain
María Villalba-Orero, María Dolores Contreras-Aguilar, Jose Joaquín Cerón, Beatriz Fuentes-Romero, Marta Valero-González, María Martín-Cuervo
Animals.2024; 14(1): 164. CrossRef - Inverse relationship between eosinophil profiles and serum glucose concentration in dogs with naturally occurring hypercortisolism
Jimin Oh, Dohee Lee, Taesik Yun, Yoonhoi Koo, Yeon Chae, Mhan-Pyo Yang, Byeong-Teck Kang, Hakhyun Kim
Domestic Animal Endocrinology.2022; 80: 106727. CrossRef - Serum Cortisol and Its Correlation with Leucocyte Profile and Circulating Lipids in Donkeys (Equus asinus)
Daniela Alberghina, Alessandra Statelli, Vincenzo Monteverde, Irene Vazzana, Giuseppe Cascone, Michele Panzera
Animals.2022; 12(7): 841. CrossRef - Changes in leukocytes and CRP in different stages of major depression
Deepti Singh, Paul C. Guest, Henrik Dobrowolny, Veronika Vasilevska, Gabriela Meyer-Lotz, Hans-Gert Bernstein, Katrin Borucki, Alexandra Neyazi, Bernhard Bogerts, Roland Jacobs, Johann Steiner
Journal of Neuroinflammation.2022;[Epub] CrossRef - HIF1α is a direct regulator of steroidogenesis in the adrenal gland
Deepika Watts, Johanna Stein, Ana Meneses, Nicole Bechmann, Ales Neuwirth, Denise Kaden, Anja Krüger, Anupam Sinha, Vasileia Ismini Alexaki, Luis Gustavo Perez-Rivas, Stefan Kircher, Antoine Martinez, Marily Theodoropoulou, Graeme Eisenhofer, Mirko Peitz
Cellular and Molecular Life Sciences.2021; 78(7): 3577. CrossRef - The Immune System in Cushing’s Syndrome
Valeria Hasenmajer, Emilia Sbardella, Francesca Sciarra, Marianna Minnetti, Andrea M. Isidori, Mary Anna Venneri
Trends in Endocrinology & Metabolism.2020; 31(9): 655. CrossRef
- Association between Eosinophil Count and Cortisol Concentrations in Equids Admitted in the Emergency Unit with Abdominal Pain

- Obesity and Metabolism
- Plasma Adiponectin Levels in Elderly Patients with Prediabetes
- Si Eun Kong, Yea Eun Kang, Kyong Hye Joung, Ju Hee Lee, Hyun Jin Kim, Bon Jeong Ku
- Endocrinol Metab. 2015;30(3):326-333. Published online August 4, 2015
- DOI: https://doi.org/10.3803/EnM.2015.30.3.326
- 3,239 View
- 36 Download
- 7 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The significance of adiponectin levels in elderly individuals with prediabetes has yet to be determined. Thus, the present study was performed to evaluate the relationships between adiponectin levels and anthropometric variables, body composition parameters, insulin sensitivity, and lipid profiles in elderly prediabetic patients.
Methods The present study included 120 subjects with prediabetes who were >65 years of age and were selected from among 1,993 subjects enrolled in the Korea Rural Genomic Cohort Study. All subjects underwent a 75 g oral glucose tolerance test and tests for measurement of insulin sensitivity. All diagnoses of prediabetes satisfied the criteria of the American Diabetes Association.
Results Plasma adiponectin levels were lower in elderly prediabetic subjects than elderly subjects with normal glucose tolerance (
P <0.01) as well as in elderly prediabetic patients with metabolic syndrome (MetS) than in those without MetS (P <0.02). When the subjects were categorized into two groups according to plasma adiponectin levels, the waist-to-hip ratio and 2-hour insulin levels were significantly lower in individuals with high plasma adiponectin levels than in those with low plasma adiponectin levels. Additionally, the plasma adiponectin levels of elderly prediabetic subject were inversely correlated with body mass index (BMI), waist circumference (WC), waist-to-hip ratio, visceral fat, visceral fat ratio, and 2-hour insulin levels.Conclusion The present findings demonstrated that the major factors correlated with adiponectin levels in elderly prediabetic subjects were BMI, WC, waist-to-hip ratio, visceral fat, visceral fat ratio, and 2-hour insulin levels.
-
Citations
Citations to this article as recorded by- Differential Association of Selected Adipocytokines, Adiponectin, Leptin, Resistin, Visfatin and Chemerin, with the Pathogenesis and Progression of Type 2 Diabetes Mellitus (T2DM) in the Asir Region of Saudi Arabia: A Case Control Study
Mohammad Muzaffar Mir, Rashid Mir, Mushabab Ayed Abdullah Alghamdi, Javed Iqbal Wani, Zia Ul Sabah, Mohammed Jeelani, Vijaya Marakala, Shahzada Khalid Sohail, Mohamed O’haj, Muffarah Hamid Alharthi, Mohannad Mohammad S. Alamri
Journal of Personalized Medicine.2022; 12(5): 735. CrossRef - Postloading insulinemia is independently associated with arterial stiffness in young Japanese persons
Norimitsu Murai, Naoko Saito, Sayuri Nii, Yuto Nishikawa, Asami Suzuki, Eriko Kodama, Tatsuya Iida, Kentaro Mikura, Hideyuki Imai, Mai Hashizume, Yasuyoshi Kigawa, Rie Tadokoro, Chiho Sugisawa, Kei Endo, Toru Iizaka, Fumiko Otsuka, Shun Ishibashi, Shoichi
Hypertension Research.2021; 44(11): 1515. CrossRef - Association of Adiponectin and rs1501299 of the ADIPOQ Gene with Prediabetes in Jordan
Mahmoud Alfaqih, Faheem Al-Mughales, Othman Al-Shboul, Mohammad Al Qudah, Yousef Khader, Muhammad Al-Jarrah
Biomolecules.2018; 8(4): 117. CrossRef
- Differential Association of Selected Adipocytokines, Adiponectin, Leptin, Resistin, Visfatin and Chemerin, with the Pathogenesis and Progression of Type 2 Diabetes Mellitus (T2DM) in the Asir Region of Saudi Arabia: A Case Control Study

- A Case of Giant Cell Granulomatous Hypophysitis with Recurrent Hypoosmolar Hyponatremia.
- Yun Hyeong Lee, Yong Bum Kim, Ju Hee Lee, Kyoung Hye Jeong, Min Kyeong Kim, Kyu Sang Song, Young Suk Jo
- Endocrinol Metab. 2010;25(4):347-353. Published online December 1, 2010
- DOI: https://doi.org/10.3803/EnM.2010.25.4.347
- 2,052 View
- 24 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - A 39-year-old woman presented with a 20 day history of recurrent hypoosmolar hyponatremia. Because her volume status seemed to be normal, the most suspected causes of her hyponatremia were adrenal insufficiency and hypothyroidism. Endocrinologic examination, including a combined pituitary function test, showed TSH and ACTH deficiency without GH deficiency, and hyperprolactinemia was also present. Sella MRI showed a pituitary mass, stalk thickening and loss of the normal neurohypophysial hyperintense signal on the T1 weighted image. Pathologic exam demonstrated granulomatous lesions and Langhans' multinucleated giant cells with inflammatory cell infiltration. After high dose methylprednisolone pulse therapy (1 g/day for 3 days) with subsequent prednisolone and levothyoxine replacement, there was no more recurrence of the hyponatremia. The sella MRI on the 6th month showed decreased mass size, narrowed stalk thickening and the reappearance of the normal neurohyphophysial hyperintense signal. She is currently in a good general condition and is receiving hormone replacement therapy.
-
Citations
Citations to this article as recorded by- Primary Granulomatous Hypophysitis Presenting with Panhypopituitarism and Central Diabetes Insipidus
Hyun Jin Oh, Ji Young Mok, Ji Eun Kim, Sung Bae Cho, Sang Ah Chang, Ji Hyun Kim, Jung Min Lee
Korean Journal of Medicine.2015; 88(5): 581. CrossRef - Idiopathic granulomatous hypophysitis: a systematic review of 82 cases in the literature
Benjamin H. M. Hunn, William G. Martin, Steven Simpson, Catriona A. Mclean
Pituitary.2014; 17(4): 357. CrossRef
- Primary Granulomatous Hypophysitis Presenting with Panhypopituitarism and Central Diabetes Insipidus


 KES
KES

 First
First Prev
Prev



